Decline In Male Infertility
Is Male Infertility Increasing?
Male infertility has always been one of the diagnoses made in couples. This can be a very elusive diagnosis given the fact that if a man has a reasonable sperm count it could be expected that fertilization of the wife's eggs should be able to take place. And indeed, nowadays with the miracles of IVF and intracytoplasmic sperm injection (ICSI) that definitely is the expectation.
One of the other complicating factors about male infertility is the controversy about what is a normal semen analysis. When I first started my training over 45 years ago, a normal sperm count was thought to be >30,000,000 sperm/cc with motility >70%. In the intervening years, the numbers that represent a normal semen analysis have been a moving target. Currently many infertility specialists feel as though the cutoff is 15,000,000 sperm/cc and 30% motility.
A study performed in 1998 looked at the association between semen quality and the probability of conception in a single menstrual cycle in Danish couples with no previous reproductive experience. The couples (430) discontinued use of contraception and were then followed for 6 menstrual cycles or until a pregnancy was identified within that 6-month window. There were 256 (59·5%) pregnancies among the 430 couples and 165 (65·0%) among those with a sperm concentration greater than 40,000,000/cc. Among those couples with a lower sperm concentration there were 84 (51·2%) pregnancies. The probability of conception increased with increasing sperm concentration up to 40,000,000/cc, and a higher sperm density was not associated with any increasing likelihood of pregnancy. This study suggested that the current guidelines for normal semen quality should be used with caution. Some men with a sperm count above the lower limit of the normal range estimate of 15,000,000 may in fact be subfertile.
The question we need to ask is why has the definition of a normal sperm count dropped so much during that time? Are sperm in 2024 better at fertilizing eggs than sperm were in 1978? I seriously doubt that that is the case and in fact there is evidence to think that not only sperm numbers but sperm quality has also decreased during the past 50 years.
One of the issues is that as with a lot of laboratory tests, the “normal” range is really looking at the average for the population and not what is truly a normal or optimal value. Frequently laboratories will determine "normal" blood test based upon the last 1000 patients who had their blood drawn for testing. This can be a biased number because people getting blood drawn are frequently people who have some kind of medical problem or complaint that compelled their doctor to perform testing. Other times laboratories will recruit so-called "normal" individuals from a presumably healthy population and utilize those numbers to define a normal value. The problem with both of these methods is that they are looking at population averages and not necessarily a value that truly denotes normal good health.
When we look at semen analyses, we are looking at the number of sperm present, their motility and the size and shapes or morphology of the sperm. The problem with the analysis is that it does not give us any information about the quality of the sperm or the ability of the sperm to fertilize an egg. Unfortunately, such a test has not yet been discovered or developed.
Have sperm counts declined? As early as 1992, some investigators felt that in fact there had been a genuine decline in sperm quality for the prior 50 years which would date back to pre-World War II. Since that time there have been numerous studies that have tried to address this question; however, because of the issues that I reviewed above it has remained controversial.
In 2017, a large study which was a meta-analysis (this is a study that attempts to combine multiple studies done in the past into a summary study) found some alarming information about the trend of decreasing semen quality in men. They reviewed the results from 185 studies done between 1973 and 2011, nearly a 40-year time span. The study looked at the sperm counts from all over the world. One of the interesting findings was that semen quality from men from United States, Europe, Australia and New Zealand have dramatically dropped whereas the semen quality from South America, Asia and Africa did not show the same decline; however, it should be noted that there were very few studies from the latter geographic locations.
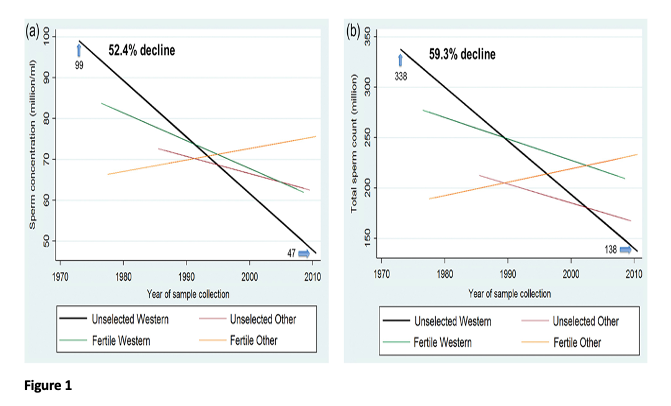
The data were separated into geographic locations and are identified as Western countries (United States, Europe, Australia and New Zealand) and Other countries which primarily included South America, Asia and Africa although as mentioned studies from these countries were limited. In the western countries sperm concentration declined by 52.4% (1.4% decline per year) and total sperm count by 59.3% (1.6% decline per year) over the years of study from 1973-2011 (see Figure 1). These declines were not changed after controlling for multiple covariates that included age, abstinence time, method of semen collection, method of sperm counting, and number of specimens per man. In addition, there was no sign of "leveling off" of the decline when the analyses were restricted to studies from 1996-2011 suggesting that semen quality is probably still decreasing at the present time.
Potential Causes of Declining Semen Quality
This study very clearly documents a decline during the past 40 years in semen quality; however, they did not attempt to address the causes for this decline. Human fertility seems to be in a downward spiral, and the science points to modern lifestyle with its technological and chemical "progress" as the likely blame. In fact, the observed changes in semen quality correspond to the rapid introduction of manmade chemicals in the post World War II era. Multiple studies have shown that developmental exposure to different types of endocrine-disrupting chemicals can dramatically have an adverse effect on reproductive development in animals. Given the increase in variety and frequency of endocrine disruptors in our environment and the adverse reproductive effects of many of these chemicals, the implications for human fertility are significant.
In a paper published in 2017, it was found that exposing male mice to the ethinyl estradiol, a synthetic estrogen found in almost all birth control pills, causes developmental problems in the reproductive tract and lowers sperm counts. The study also confirmed that estrogen exposure has generational effects. Male mice were successively less fertile with each passing generation. They observed adverse effects starting in the first generation of mouse lineages where each generation was exposed to estrogen for a brief period shortly after birth. Both reproductive tract abnormalities and decreased spermatogenesis were seen. The impacts worsened in the second generation compared to the first, and by the third generation the scientists were finding that some animals could not produce sperm at all.
Interestingly, when the first generation was exposed and the third generation was exposed even when the second generation was not exposed, the adverse reproductive effects were seen in the third generation. This suggests that the first-generation epigenetic effects of estrogen exposure are passed to the third generation without any exposure to estrogen in the second generation. This suggests that over multiple generations through germline epigenetic modifications, there may be cumulative disruption in fertility potential.
While men do not use birth control pills, they are exposed to these hormones through environmental contamination including contaminated water and as infants contaminated breastmilk if their mothers are on oral contraceptives. It is very common for women after delivery to go on birth control pills as a means of birth control and family spacing.
Men are also exposed to a number of other endocrine-disrupting chemicals in their day-to-day lives, that include endocrine-disrupting chemicals present in plastics, personal care products, and food due to contamination with herbicides such as glyphosate (Roundup) which is a very common contaminant in nonorganic foods.
While women are also adversely affected by these kinds of chemicals, men may be disproportionately affected due to the way the male reproductive system develops in utero. In early embryo development, the reproductive tracts in male and female fetuses are nearly identical. Sex hormones and specifically testosterone are what drive the differentiation between the sexes. However, when synthetic chemicals that mimic these naturally occurring hormones (endocrine-disrupting chemicals) are present, they interfere with the biological process of turning the fetus into a male.
The United States permits more than 84,000 chemicals to be used in household products, cosmetics, food and food packaging, and a majority of these have never been tested for safety. According to the U.S. Government Accountability Office, 85% of new chemical applications include no testing whatsoever.
Everything an expectant mother takes into her body can potentially get passed along to her developing child, and scientific evidence strongly suggests exposure to chemicals is contributing to cancer, reproductive abnormalities, early puberty and a host of other endocrine, neurological and metabolic problems. In a 2005 study, the Environmental Working Group (EWG) found an average of nearly 200 industrial chemicals and pollutants in the umbilical cord blood of infants born in the U.S. A total of 287 different chemicals from pesticides, consumer products, food packaging and environmental waste, including BPA, flame retardants, PCBs and even DDT have been found in cord blood.
In 2013, the EWG identified 12 of the most troublesome hormone disruptors. Surprisingly, along with some very well-known endocrine disruptors, the review also identified several you might not normally associate with hormone disruption, such as lead, mercury and arsenic. This list includes bisphenol-a (BPA), phthalates, perfluorinated chemicals (PFCs), organophosphate pesticide, dioxin, atrazine, fire retardants, perchlorate, glycol ethers, lead, mercury and arsenic.
Because many of these endocrine disruptors were not even present until post World War II, not very many human generations have gone by. This fact coupled with the information that there has been no "leveling-off" of the decline in semen quality leads to the concern that fertility in humans may continue to decline all the way to zero. Is the human species destined to extinction!!
Health Implications of Declining Semen Quality
What are the implications of the decline in semen quality? As it turns out declines in semen quality have implications beyond fertility and reproduction. These declines have been associated with the trend for increased testicular tumors, cryptorchidism (undescended testicle), and total testosterone levels. In addition, there are some public health implications as there are studies that show that poor sperm count is associated with an increase in overall morbidity and mortality in men. It is not clear that the decreased sperm count is responsible for the increase in mortality and men; however, it is more likely that they share a similar causation. Sperm counts have been associated with multiple environmental and lifestyle influences. In particular, endocrine disruption from chemical exposures may be a major factor. This may occur both prenatally and in adult life. Maternal smoking during the critical window of male reproductive development may play a role in prenatal life. Endocrine disruptors such as pesticides and plastics may play a role in both prenatal and adult life. Thus a decline in sperm count might be considered as the "canary in the coal mine" for male health.
A study performed by the Copenhagen Sperm Analysis Laboratory from 1963 to 2001 gathered information on all cases of cancer, causes of death, and number of children. Among 43,277 men without azoospermia, mortality decreased as the sperm concentration increased up to a threshold of 40,000,000/cc. As the percentage of motile and morphologically normal sperm increased, mortality decreased in a linear fashion. This decrease occurred in both men with and without children, and therefore, could not be attributed to fertility status only to semen analysis results. The size of this study lends considerable credibility to the fact that semen quality may be correlated to overall male health.
A more recent study performed in the United States involving 12,000 men showed that men seeking fertility care had a lower mortality rate than the general population. Their explanation for the overall better mortality rate for infertile man was that they were of higher social economic status and married. Both of these demographic parameters are associated with a reduced mortality rate.
However, they did find that when they stratified the men as to having normal semen analyses versus abnormal semen analyses, the mortality rate in the men with abnormal semen analyses was twice as high as those with normal semen analyses. In addition, they found that men with 2 or more abnormalities in their semen analysis had an even greater risk of mortality (see Figure 2).
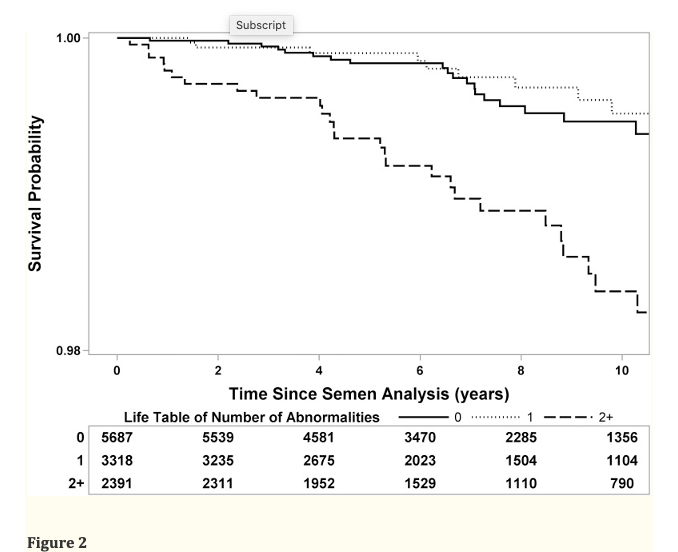
Kaplan–Meier curve of survival following semen analysis for infertile men (stratified by number of semen abnormalities: volume <1.5 ml, concentration <15 M/ml, motility <40%). Group 1: No semen abnormalities (i.e. no male factor infertility) (solid line), Group 2: One semen abnormality (dotted line), Group 3: Two or more semen abnormalities (dashed line). Survival table at bottom represents number of men available for analysis at each time point.
We might question why there might be a relationship between male fertility and mortality. Up to 15% of the man's genome is devoted to reproduction. It is likely that other nonprocreative processes may also be affected by aberrations in fertility. Defects in DNA repair will impair both meiosis and mitosis thus affecting spermatogenesis and increasing the likelihood of carcinogenesis. Hormonal aberrations may also explain the association between reduced fertility and mortality. Lower androgen levels have been linked to both infertility and cardiovascular mortality. Finally, there may be a shared risk factor etiology through lifestyle characteristics. Examples include nutrition/diet which is related to obesity and cardiovascular disease and thereby to fertility and cardiovascular disease. Smoking impacts both fertility and mortality primarily through cardiovascular disease and lung cancer. Therefore, a common etiology may be present causing both impaired overall health and reproductive health.
Take-Home Messages
1. Most importantly, men with an abnormal semen analysis do not need to think that they can never be a father. With in vitro fertilization and intracytoplasmic sperm injection, as long as a man has enough sperm to isolate some from the semen specimen, we can inseminate a woman's eggs. If she produces a dozen eggs, all we need is 12 sperm from the man. We do not need 15 or 20 or 30 million sperm.
2. Secondly, men with abnormal semen analyses should not panic and think that they will have a premature death; however, they should look at what toxic exposures and lifestyle changes they can make to improve their overall health and possibly reduce both their fertility impairment and improve their mortality.
3. Thirdly, as consumers of products and foods, we have the responsibility to dictate to large corporations the kind of products and foods that we wish to buy. If we send the message to corporations that we will not tolerate products that will contaminate our environment and adversely impact our personal health and reproductive health, corporations will respond by providing healthier options.








